Seizure in pregnancy
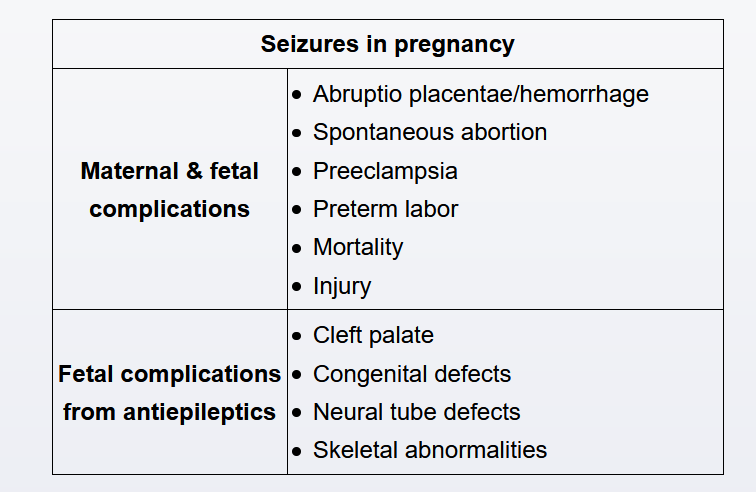
Women with epilepsy are at increased risk for obstetric complications, including preeclampsia, preterm labor, and abruptio placentae. Antiepileptic drug (AED) use is also associated with an increased risk of congenital abnormalities, including neural tube defects, congenital heart anomalies, and cleft palate. Despite these risks, the majority of women with epilepsy have a normal pregnancy.
Valproate carries the highest teratogenicity risk of all AEDs; therefore, changing to an alternate regimen should be tried 6 months prior to attempts to conceive. It is preferable to switch to the lowest possible dose of a single medication to limit teratogenicity. However, no changes to the AED regimen should be made after conception, as abrupt changes may trigger seizure activity. Gradually changing the patient's regimen by overlapping medications in early gestation exposes the fetus to possible additional teratogens. In addition, there is likely little benefit to changes in medication once pregnancy is confirmed, as the majority of organogenesis has already occurred.
Management of patients on AEDs includes initiating high-dose folic acid supplementation and screening for congenital anomalies (eg, neural tube defects) with serum alpha-fetoprotein and an anatomy ultrasound. If major abnormalities are present, pregnancy termination may be considered (Choice E).